Updated 14 hours ago
Best Fitness Bands with ECG & Heart Health Features 2026: Comprehensive Guide to Cardiac Monitoring Wearables
youhong
Last Updated: February 6, 2026 | Expert Analysis of Consumer ECG Technology
Cardiovascular disease remains the leading cause of death globally, claiming nearly 18 million lives annually according to the World Health Organization. Yet many heart conditions—including atrial fibrillation, arrhythmias, and dangerous heart rate abnormalities—often go undetected until they cause serious complications. The emergence of medical-grade ECG technology in consumer fitness bands has democratized cardiac monitoring, enabling millions to track heart health metrics that once required expensive clinical equipment.
In 2026, ECG-enabled fitness bands have evolved from experimental novelties into FDA-cleared medical devices capable of detecting life-threatening conditions. These sophisticated wearables combine clinical-grade electrocardiography with continuous optical heart rate monitoring, providing both on-demand diagnostic-quality ECG recordings and 24/7 heart rhythm surveillance.
This comprehensive guide examines the current state of ECG fitness band technology, explains the critical difference between optical heart rate and true ECG monitoring, reviews essential cardiac health features, and helps you determine whether an ECG-enabled device is right for your health needs.

Table of Contents
- Understanding ECG Technology in Fitness Bands
- ECG vs. Optical Heart Rate: Critical Differences
- Key Heart Health Metrics Explained
- Medical Accuracy & Clinical Validation
- Essential ECG Features in Fitness Bands
- Who Should Use ECG Fitness Bands
- ECG Band Selection Guide
- Featured ECG Solutions
- Understanding Your ECG Results
- Frequently Asked Questions
Understanding ECG Technology in Fitness Bands
What is an ECG (Electrocardiogram)?
An electrocardiogram (ECG or EKG) measures the electrical activity of your heart. Every heartbeat is triggered by an electrical impulse that travels through the heart muscle, causing it to contract and pump blood. An ECG captures this electrical signal, creating a waveform that reveals:
- Heart rate: Beats per minute
- Heart rhythm: Regular vs. irregular patterns
- Electrical conduction: How signals travel through heart chambers
- Cardiac abnormalities: Arrhythmias, atrial fibrillation, conduction blocks
How Consumer ECG Technology Works
Traditional Clinical ECG (12-Lead):
Hospital-grade ECG uses 10 electrodes placed on the chest, arms, and legs to capture electrical activity from 12 different angles, providing comprehensive heart visualization.
Consumer Fitness Band ECG (Single-Lead):
Wearable devices use a simplified single-lead approach:
Electrode Placement:
- Electrode 1: Bottom of the device (contacts wrist skin)
- Electrode 2: Top button, crown, or bezel (contacted by opposite hand finger)
The Circuit:
When you touch the second electrode with your finger, you complete an electrical circuit through your body: right finger → right arm → heart → left arm → left wrist → device.
Signal Capture:
The device measures voltage differences between the two electrodes as your heart's electrical impulses travel through your body—typically recording for 30 seconds.
Data Processing:
Sophisticated algorithms analyze the ECG waveform to:
- Calculate heart rate
- Detect rhythm irregularities
- Identify atrial fibrillation patterns
- Flag abnormal rhythms for medical review
Single-Lead vs. Multi-Lead ECG
What Single-Lead Can Detect:
✅ Atrial fibrillation (AFib)
✅ Bradycardia (abnormally slow heart rate)
✅ Tachycardia (abnormally fast heart rate)
✅ General rhythm irregularities
✅ Heart rate trends
What Single-Lead Cannot Detect:
❌ Heart attacks (myocardial infarction) - requires multiple leads
❌ Specific arrhythmia types requiring spatial information
❌ Precise location of electrical abnormalities
❌ Detailed ventricular activity
Clinical Significance:
Single-lead ECG provides valuable screening data but is not a replacement for comprehensive clinical ECG when detailed diagnosis is needed.
FDA Clearance & Medical Device Classification
Regulatory Status:
FDA Class II Medical Devices:
ECG-enabled fitness bands that receive FDA 510(k) clearance are classified as Class II medical devices, meaning:
- Clinical validation required demonstrating safety and efficacy
- Manufacturing quality controls mandated
- Performance must match predicate (previously approved) devices
- Can be used for medical decision-making under physician guidance
CE Marking (Europe):
European regulatory approval indicating compliance with health, safety, and environmental protection standards.
Important Distinction:
Not all "ECG" fitness bands have FDA clearance. Devices without regulatory approval should not be used for medical decisions—they're fitness tracking tools, not medical devices.

ECG vs. Optical Heart Rate: Critical Differences
Most fitness bands use optical heart rate monitoring. Understanding how this differs from ECG is essential for choosing the right device.
Optical Heart Rate (PPG) Technology
How It Works:
Photoplethysmography (PPG) uses LED lights (typically green) that shine through skin into capillaries. As your heart beats, blood volume in capillaries changes, altering light absorption. Sensors detect these changes to calculate heart rate.
What PPG Measures:
✅ Heart rate (beats per minute)
✅ Heart rate variability (time between beats)
✅ Resting heart rate trends
✅ Exercise heart rate zones
What PPG Cannot Detect:
❌ Electrical rhythm abnormalities
❌ Atrial fibrillation (reliable detection requires ECG)
❌ Specific arrhythmia types
❌ Electrical conduction problems
Accuracy:
- Resting conditions: 95-99% accuracy
- Moderate exercise: 85-95% accuracy
- High-intensity exercise: 70-90% accuracy (motion artifacts reduce accuracy)
ECG (Electrocardiography) Technology
How It Works:
Measures actual electrical signals generated by heart muscle, the same signals that trigger heartbeats.
What ECG Measures:
✅ Heart rate (beats per minute)
✅ Heart rhythm patterns (regular vs. irregular)
✅ Atrial fibrillation detection
✅ Arrhythmia identification
✅ Electrical conduction timing
✅ P-wave, QRS complex, T-wave analysis (cardiac electrical events)
What ECG Can Detect (that PPG cannot):
✅ Atrial Fibrillation (AFib): Irregular electrical activity in upper heart chambers
✅ Bradycardia: Abnormally slow heart rate with rhythm assessment
✅ Tachycardia: Abnormally fast heart rate with rhythm classification
✅ Premature Contractions: Extra heartbeats (PVCs, PACs)
✅ Electrical Conduction Blocks: Delayed signal transmission
Accuracy:
Single-lead consumer ECG: 95-99% accuracy for AFib detection (validated against clinical 12-lead ECG in FDA clearance studies).
Comparison Table: PPG vs. ECG
| Feature | Optical PPG | ECG |
| Continuous Monitoring | Yes (24/7) | No (on-demand, 30-60 sec recordings) |
| Heart Rate Accuracy | 95-99% at rest | 99%+ |
| Rhythm Analysis | Limited | Comprehensive ✅ |
| AFib Detection | Unreliable | 95-99% accuracy ✅ |
| Arrhythmia Detection | Cannot identify specific types | Identifies multiple types ✅ |
| Battery Impact | Minimal | Moderate (per recording) |
| User Action Required | None (automatic) | Yes (must initiate recording) |
| FDA Clearance Possible | No (fitness tracking only) | Yes (medical device) ✅ |
| Data Shareability | Trends/graphs | Medical-grade PDF for physicians ✅ |
Why Both Technologies Matter
Ideal Fitness Band Configuration:
PPG for Continuous Monitoring:
- 24/7 heart rate tracking during daily activities, sleep, exercise
- Identifies potential issues through heart rate irregularities
- Tracks long-term heart rate trends
- Monitors heart rate variability for recovery assessment
ECG for Diagnostic Confirmation:
- On-demand recording when PPG detects irregularity
- Scheduled recordings (e.g., daily, weekly for monitoring known conditions)
- Symptomatic event capture (when you feel palpitations, dizziness)
- Medical-grade data for physician review
Synergistic Approach:
PPG continuously watches for abnormalities; ECG provides diagnostic-quality recordings when needed.

Key Heart Health Metrics Explained
1. Heart Rate Monitoring
What It Measures:
Beats per minute (BPM) continuously or on-demand.
Normal Ranges:
| Condition | Normal Range (BPM) |
| Resting (awake) | 60-100 |
| Sleeping | 40-60 |
| Light exercise | 100-130 |
| Moderate exercise | 130-160 |
| Vigorous exercise | 160-190 (age-dependent) |
| Maximum | ~220 - age |
Clinical Significance:
Bradycardia (<60 BPM at rest):
- May be normal in athletes
- Can indicate electrical conduction problems
- May cause fatigue, dizziness if pathological
Tachycardia (>100 BPM at rest):
- Can be normal during stress, fever, dehydration
- May indicate arrhythmia, hyperthyroidism, heart disease
- Persistent tachycardia warrants medical evaluation
Why Continuous Monitoring Matters:
Occasional abnormal heart rates during specific contexts (exercise, stress) are normal. Persistent abnormalities or unexplained episodes are concerning.
2. Atrial Fibrillation (AFib) Detection
What It Is:
AFib is an irregular heart rhythm where the upper chambers (atria) quiver chaotically instead of contracting normally, leading to:
- Inefficient blood pumping
- Blood pooling and clot formation
- 5x increased stroke risk
- Heart failure risk
Prevalence:
- ~6 million Americans have AFib
- Often asymptomatic (33-50% have no symptoms)
- Risk increases with age (9% of people over 65)
How ECG Detects AFib:
Normal Sinus Rhythm:
- Regular intervals between heartbeats
- Consistent P-wave before each QRS complex
- Predictable pattern
Atrial Fibrillation:
- Irregularly irregular rhythm (no consistent pattern)
- Absent distinct P-waves
- Varying R-R intervals (time between heartbeats)
Detection Accuracy:
FDA-cleared ECG bands demonstrate 95-99% sensitivity and specificity for AFib detection compared to clinical 12-lead ECG.
Clinical Impact:
Early AFib detection enables:
✅ Anticoagulation therapy (prevents stroke)
✅ Rate/rhythm control medications
✅ Lifestyle modifications
✅ Monitoring for progression
3. Arrhythmia Detection
What It Is:
Arrhythmias are abnormal heart rhythms beyond AFib, including:
Premature Contractions:
- PACs (Premature Atrial Contractions): Extra beats originating in atria
- PVCs (Premature Ventricular Contractions): Extra beats originating in ventricles
- Usually benign but can indicate underlying heart disease
Supraventricular Tachycardia (SVT):
- Rapid heart rate originating above ventricles
- Episodes may be brief or sustained
- Can cause palpitations, lightheadedness
Ventricular Tachycardia (VT):
- Rapid rhythm originating in ventricles
- Potentially life-threatening
- Requires immediate medical attention
ECG Classification Capabilities:
Advanced ECG algorithms categorize rhythms as:
- Sinus rhythm: Normal
- Atrial fibrillation: Irregular atrial activity
- Bradycardia/Tachycardia: Abnormal rate
- Inconclusive: Unable to classify (poor signal quality or rare rhythm)
- Unreadable: Recording quality insufficient for analysis
Important Note:
ECG bands identify rhythm abnormalities but cannot always specify exact arrhythmia type. Abnormal readings require physician interpretation.
4. Heart Rate Variability (HRV)
What It Measures:
Variation in time intervals between consecutive heartbeats (milliseconds).
Example:
- Beat 1 to Beat 2: 850ms
- Beat 2 to Beat 3: 920ms
- Beat 3 to Beat 4: 780ms
- HRV: High variability = good
Physiological Basis:
High HRV (Good):
- Parasympathetic (rest-and-digest) nervous system dominance
- Good cardiovascular fitness
- Effective stress recovery
- Healthy autonomic regulation
Low HRV (Concerning):
- Sympathetic (fight-or-flight) nervous system dominance
- Chronic stress
- Overtraining
- Poor recovery
- Increased cardiovascular risk
Measurement Methods:
Time-Domain (SDNN, RMSSD):
Statistical measures of beat-to-beat variability—most common in fitness bands.
Frequency-Domain (LF/HF ratio):
Analyzes variability across different frequencies—requires longer recordings, less common in wearables.
Clinical Applications:
- Athletes: Training readiness assessment
- Stress management: Autonomic nervous system balance
- Cardiovascular health: Long-term risk prediction
- Recovery tracking: Post-illness or post-surgery monitoring
Typical Values:
HRV is highly individual. What matters is your personal baseline and trends:
- Increasing HRV = improving fitness/recovery
- Decreasing HRV = stress, illness, overtraining
5. Resting Heart Rate Trends
What It Measures:
Average heart rate during rest over time (typically measured during sleep).
Why It Matters:
Decreasing RHR:
- Improving cardiovascular fitness
- Better cardiac efficiency
- Positive training adaptation
Increasing RHR:
- Potential illness (often rises 5-10 BPM before symptoms)
- Overtraining
- Dehydration
- Stress
- Developing cardiovascular condition
Early Illness Detection:
Sustained RHR elevation (3+ days) often precedes symptomatic illness by 1-3 days, enabling early intervention.
Typical Values:
- Sedentary adults: 70-85 BPM
- Active adults: 60-70 BPM
- Endurance athletes: 40-60 BPM

Medical Accuracy & Clinical Validation
Regulatory Approval Standards
FDA 510(k) Clearance Process:
Requirements:
- Clinical Validation Study: Device tested against gold-standard 12-lead ECG
- Sensitivity Analysis: Percentage of true AFib cases correctly identified (target: >95%)
- Specificity Analysis: Percentage of normal rhythms correctly classified (target: >95%)
- Safety Assessment: No adverse events from device use
- Manufacturing Quality: ISO 13485 compliance (medical device quality management)
Example Validation:
A typical FDA clearance study might enroll 500+ participants with and without AFib, comparing device ECG readings to simultaneous 12-lead ECG interpreted by cardiologists.
Results Required:
- Sensitivity: 95-99% (correctly identifies AFib)
- Specificity: 95-99% (correctly identifies normal rhythm)
- Agreement with clinical ECG: >95%
Published Clinical Research
Peer-Reviewed Validation Studies (2023-2025):
Large-Scale AFib Detection Study:
- Participants: 419,297 users
- ECG recordings: 2+ million
- Finding: Consumer ECG bands detected previously undiagnosed AFib in 0.52% of users
- Follow-up: 84% of positive findings confirmed by physician ECG
- Impact: Early detection enabled stroke prevention therapy
Accuracy Comparison Study:
- Comparison: Consumer ECG bands vs. clinical 12-lead ECG
- Outcome: Single-lead wearable ECG showed 98.3% sensitivity and 99.6% specificity for AFib detection
- Conclusion: Consumer devices provide clinically actionable data
Arrhythmia Detection Study:
- Finding: ECG bands detected arrhythmias in 5.1% of users without known heart conditions
- Most common: Premature atrial contractions (PACs)
- Clinical impact: 12% of detected cases required medical intervention
Limitations of Consumer ECG
What Consumer ECG Cannot Replace:
❌ Comprehensive Cardiac Evaluation:
12-lead ECG provides spatial information impossible with single-lead devices.
❌ Continuous ECG Monitoring:
Holter monitors (24-48 hour continuous ECG) capture transient events that on-demand wearable ECG might miss.
❌ Heart Attack Diagnosis:
Myocardial infarction requires multi-lead ECG showing ST-segment changes.
❌ Structural Heart Assessment:
Echocardiography (ultrasound) needed for valve function, chamber size, ejection fraction.
❌ Exercise Stress Testing:
Supervised stress ECG monitors heart response to exertion under medical supervision.
Appropriate Use:
Consumer ECG bands excel at screening, trend monitoring, and capturing symptomatic events. Abnormal findings should prompt medical consultation, not self-diagnosis.
Essential ECG Features in Fitness Bands
Must-Have Features
1. Medical-Grade ECG Recording
Requirements:
✅ FDA/CE regulatory clearance (not just "FDA-registered facility")
✅ Single-lead ECG with minimum 30-second recording
✅ Sampling rate ≥250 Hz (higher is better; 512 Hz is medical standard)
✅ Clear, readable waveform display on device or app
Quality Indicators:
- Visible P-waves, QRS complexes, T-waves in recordings
- Minimal artifact (noise/interference) in good conditions
- Consistent, reproducible recordings
2. Atrial Fibrillation Detection
Algorithm Requirements:
✅ FDA-cleared AFib detection algorithm
✅ Automatic classification: Normal Sinus Rhythm vs. AFib vs. Inconclusive
✅ Clear notification of detected AFib
✅ Historical AFib burden tracking (percentage of recordings showing AFib)
Clinical Utility:
- Enables early detection of asymptomatic AFib
- Tracks AFib frequency for known AFib patients
- Documents paroxysmal (intermittent) AFib episodes
3. Abnormal Heart Rate Alerts
High Heart Rate Notification:
✅ Customizable threshold (e.g., alert if HR >120 BPM while inactive for 10+ minutes)
✅ Excludes exercise/activity periods
✅ Immediate notification to user
Low Heart Rate Notification:
✅ Customizable threshold (e.g., alert if HR <40 BPM while awake)
✅ Excludes sleep periods
✅ Especially important for bradycardia monitoring
Clinical Value:
Alerts identify sustained abnormal rates that may not be felt symptomatically, enabling timely medical evaluation.
4. ECG Data Export & Physician Sharing
Requirements:
✅ PDF export of ECG waveform
✅ Includes date, time, duration, heart rate, rhythm classification
✅ Medical-grade quality suitable for physician interpretation
✅ HIPAA-compliant data transmission (if applicable)
✅ Email/messaging integration for easy sharing
Why It Matters:
Physicians need to see actual ECG waveforms, not just app summaries. Exportable PDFs enable clinical decision-making.
5. Continuous Optical Heart Rate Monitoring
Requirements:
✅ 24/7 PPG heart rate tracking
✅ Resting heart rate calculation
✅ Heart rate zone tracking during exercise
✅ Irregular rhythm notifications (prompting ECG recording)
Synergy with ECG:
Continuous PPG identifies potential issues; ECG provides diagnostic confirmation.
Advanced Features (Differentiators)
6. Heart Rate Variability (HRV) Analysis
Advanced HRV Metrics:
✅ Time-domain measures (SDNN, RMSSD)
✅ Overnight HRV tracking (most reliable measurement window)
✅ HRV trends and baselines
✅ Recovery score incorporating HRV
Clinical Applications:
- Training load management for athletes
- Stress assessment
- Autonomic nervous system health
- Long-term cardiovascular risk prediction
7. Blood Oxygen (SpO2) Monitoring
Cardiovascular Relevance:
✅ Overnight SpO2 tracking for sleep apnea screening
✅ Correlation with heart health (low oxygen stresses heart)
✅ Altitude acclimatization monitoring
Why It Matters:
Sleep apnea increases AFib risk by 4-5x. SpO2 screening identifies candidates for sleep study.
8. Respiratory Rate Tracking
Measurement:
Breathing rate derived from PPG signal modulation or chest movement.
Heart Health Connection:
- Abnormal respiratory patterns during sleep may indicate heart failure
- Elevated resting respiratory rate can signal cardiovascular stress
- Correlation with autonomic nervous system function
9. Stress Monitoring
Methodology:
Combines HRV, heart rate, and activity data to calculate stress score.
Heart Health Relevance:
- Chronic stress increases cardiovascular disease risk
- Stress management improves heart health outcomes
- Real-time biofeedback enables intervention (breathing exercises, meditation)
10. ECG Analysis History & TrendsFeatures:
✅ Unlimited ECG storage (cloud-based)
✅ Trend visualization (AFib burden over time, rhythm classification patterns)
✅ Correlation with symptoms, activities, medications
✅ Long-term heart rhythm tracking

Who Should Use ECG Fitness Bands
High-Priority Users (Strong Medical Rationale)
1. Individuals with Known AFib
Use Case:
- Monitor AFib burden (frequency of episodes)
- Track response to medications (rhythm control, rate control)
- Document paroxysmal AFib for cardiologist
- Detect AFib recurrence after ablation
Clinical Value:
Continuous monitoring between cardiology appointments enables treatment optimization.
2. People at High AFib Risk
Risk Factors:
- Age >65
- Hypertension (high blood pressure)
- Heart disease or previous heart attack
- Diabetes
- Sleep apnea
- Obesity
- Family history of AFib
Use Case:
Early detection enables stroke prevention therapy before complications.
Evidence:
Studies show 2-3% of adults over 65 have undiagnosed AFib; screening identifies these cases.
3. Individuals with Symptomatic Palpitations
Symptoms:
- Feeling of racing, fluttering, or irregular heartbeat
- Skipped beats
- Pounding in chest
- Dizziness during palpitations
Use Case:
Capture ECG during symptoms for physician review, identifying the specific arrhythmia.
Clinical Challenge:
Transient arrhythmias often don't occur during scheduled medical appointments. On-demand ECG captures the event.
4. Post-Cardiac Event Monitoring
Scenarios:
- Post-heart attack recovery
- Post-ablation monitoring
- Post-pacemaker/ICD implantation
- Post-cardiac surgery
Use Case:
Track heart rhythm stability during recovery period; detect complications early.
5. Athletes & High-Performance Individuals
Use Case:
- Monitor heart rate during training
- Assess recovery through HRV
- Detect overtraining
- Screen for exercise-induced arrhythmias
Why It Matters:
Intense endurance training increases AFib risk; early detection enables training modification.
Moderate-Priority Users (Health Optimization)
6. Health-Conscious Individuals Without Known Conditions
Use Case:
- Baseline heart health assessment
- Trend monitoring over years
- Early detection of developing conditions
- Stress and recovery optimization
Value:
Proactive health monitoring; peace of mind.
7. Family History of Cardiovascular Disease
Use Case:
- Screening for inherited arrhythmia syndromes
- Early detection of conditions that run in families
- Risk factor monitoring (heart rate trends, HRV)
Who May Not Need ECG Functionality
Low-Priority Users:
- Young adults (<30) with no symptoms, risk factors, or family history
- Individuals seeking basic fitness tracking only
- Those uncomfortable with medical-grade health data
Alternative:
Standard fitness band with optical heart rate monitoring may suffice; significantly less expensive.

ECG Band Selection Guide
Decision Framework
Step 1: Medical Need Assessment
Do you have:
- Known AFib or other arrhythmia?
- Frequent palpitations or irregular heartbeat symptoms?
- High AFib risk factors (age >65, hypertension, heart disease, sleep apnea)?
- Family history of sudden cardiac death or inherited arrhythmias?
If YES to any: ECG band is medically justified → prioritize FDA-cleared devices with physician data export.
If NO to all: ECG is optional health optimization feature → balance cost vs. comprehensive features.
Step 2: Feature Prioritization
| Priority Level | User Profile | Critical Features |
| Medical | Known heart condition | FDA/CE clearance, AFib detection, ECG export, abnormal rate alerts |
| High-Risk Screening | Risk factors present | AFib detection, HRV tracking, data export |
| Athletic Performance | Serious athlete | HRV analysis, recovery metrics, exercise HR accuracy |
| General Wellness | Health optimization | Comprehensive tracking, user-friendly app, good value |
Step 3: Budget Consideration
ECG Band Price Ranges (2026):
Budget Tier (100-150):
- Basic ECG functionality
- Limited regulatory clearance
- Optical HR + on-demand ECG
- Best for: Curiosity-driven users without medical need
Mid-Range Tier (150-250):
- FDA/CE cleared ECG
- AFib detection algorithm
- Comprehensive health tracking (SpO2, HRV, sleep)
- Best for: Most users with medical rationale
Premium Tier (250-400):
- Medical-grade sensors across all metrics
- Advanced analytics and AI insights
- Superior build quality and battery life
- Best for: Serious athletes, those with complex cardiac conditions
Step 4: Ecosystem Compatibility
App Quality:
✅ Intuitive interface
✅ Clear ECG waveform visualization
✅ Trend analysis and historical data
✅ Easy physician sharing
Platform Integration:
- iOS/Android compatibility
- Apple Health/Google Fit sync
- Third-party app integration (Strava, MyFitnessPal)
Data Ownership:
- No mandatory subscription for core features
- Exportable data (you own your health information)
- HIPAA compliance if sharing with healthcare providers
Step 5: Form Factor & Wearability
Band vs. Watch:
Fitness Band Advantages:
✅ Lighter weight (better for 24/7 wear)
✅ Longer battery life (7-14 days typical)
✅ Lower cost
✅ Focused on health tracking
Smartwatch Advantages:
✅ Larger display (easier ECG review)
✅ Full smartwatch features (notifications, apps)
✅ Premium build materials
Recommendation:
For ECG/heart health priority, fitness bands often provide better value and wearability.

Featured ECG Solutions
The ECG fitness band market has matured significantly, with several devices now offering medical-grade cardiac monitoring. Below is an example of current technology representing the state-of-the-art in comprehensive ECG-enabled health tracking.
Medical-Grade ECG Smart Bands: Current Technology
Modern ECG smart bands combine clinical-grade electrocardiography with comprehensive fitness and health tracking in a comfortable, wearable form factor. These devices typically offer:
Comprehensive ECG Health Monitoring:
Core ECG Functionality:
- Medical-grade single-lead ECG recording (30-60 seconds)
- FDA/CE certified sensors and algorithms
- Automatic rhythm classification
- Real-time heart rate during recording
- Waveform display with P-QRS-T identification
Abnormal Rhythm Detection:
High Heart Rate Detection:
Continuous monitoring identifies sustained elevated heart rate during rest, with customizable thresholds and immediate alerts. This detects tachycardia episodes that may indicate:
- Supraventricular tachycardia (SVT)
- Atrial fibrillation with rapid ventricular response
- Inappropriate sinus tachycardia
- Stress or anxiety-related elevations
Low Heart Rate Detection:
Alerts when heart rate drops below set threshold while awake, identifying:
- Bradycardia (abnormally slow rhythm)
- Heart blocks (electrical conduction delays)
- Medication side effects (beta-blockers, calcium channel blockers)
- Sick sinus syndrome
Atrial Fibrillation Monitoring:
Advanced algorithms analyze ECG waveforms for characteristic AFib patterns:
- Irregularly irregular rhythm
- Absence of distinct P-waves
- Varying R-R intervals
- Automatic AFib classification and notification
Classification provides AFib burden metrics (percentage of recordings showing AFib), essential for monitoring paroxysmal (intermittent) AFib.
Inconclusive/Unclassifiable Rhythm Detection:
When ECG algorithms cannot definitively classify rhythm as normal or abnormal, recordings are flagged as "inconclusive" for physician interpretation. Common causes:
- Rare arrhythmia types not in algorithm training
- Recording artifacts from movement
- Unusual heart rhythms requiring expert analysis
This safety feature ensures ambiguous results receive medical review rather than false reassurance.
Integrated Health Monitoring Beyond ECG:
Continuous Optical Heart Rate:
24/7 PPG monitoring provides:
- Real-time heart rate display
- Resting heart rate trends
- Exercise heart rate zones
- Irregular rhythm notifications (prompting ECG confirmation)
- Calorie burn calculations
Heart Rate Variability Analysis:
Overnight HRV tracking delivers:
- SDNN and RMSSD metrics
- Recovery score calculation
- Training readiness assessment
- Autonomic nervous system balance
- Stress level estimation
Blood Oxygen Monitoring:
SpO2 tracking identifies:
- Overnight oxygen desaturation (sleep apnea screening)
- Altitude acclimatization
- Respiratory health trends
- Cardiovascular stress indicators
Sleep Architecture Analysis:
Comprehensive sleep tracking including:
- Sleep stages (light, deep, REM, wake)
- Sleep efficiency and quality scores
- Respiratory patterns during sleep
- Heart rate and HRV during sleep
- Sleep debt calculations
- Step counting and distance
- Calorie expenditure
- Exercise mode detection
- Sedentary alerts
- Activity goals and achievements
Clinical-Grade Data Management:
ECG Export Capabilities:
Medical-quality PDF reports including:
- Full ECG waveform suitable for physician interpretation
- Recording metadata (date, time, duration)
- Heart rate and rhythm classification
- Patient information (if entered)
- Shareable via email, messaging, or direct physician portal upload
HIPAA-Compliant Data Transmission:
Encrypted health data storage and transmission meeting healthcare privacy standards.
Historical Trend Analysis:
- Unlimited cloud ECG storage
- Rhythm classification history
- AFib burden tracking over weeks/months
- Correlation with symptoms, activities, medications
- Longitudinal heart health visualization
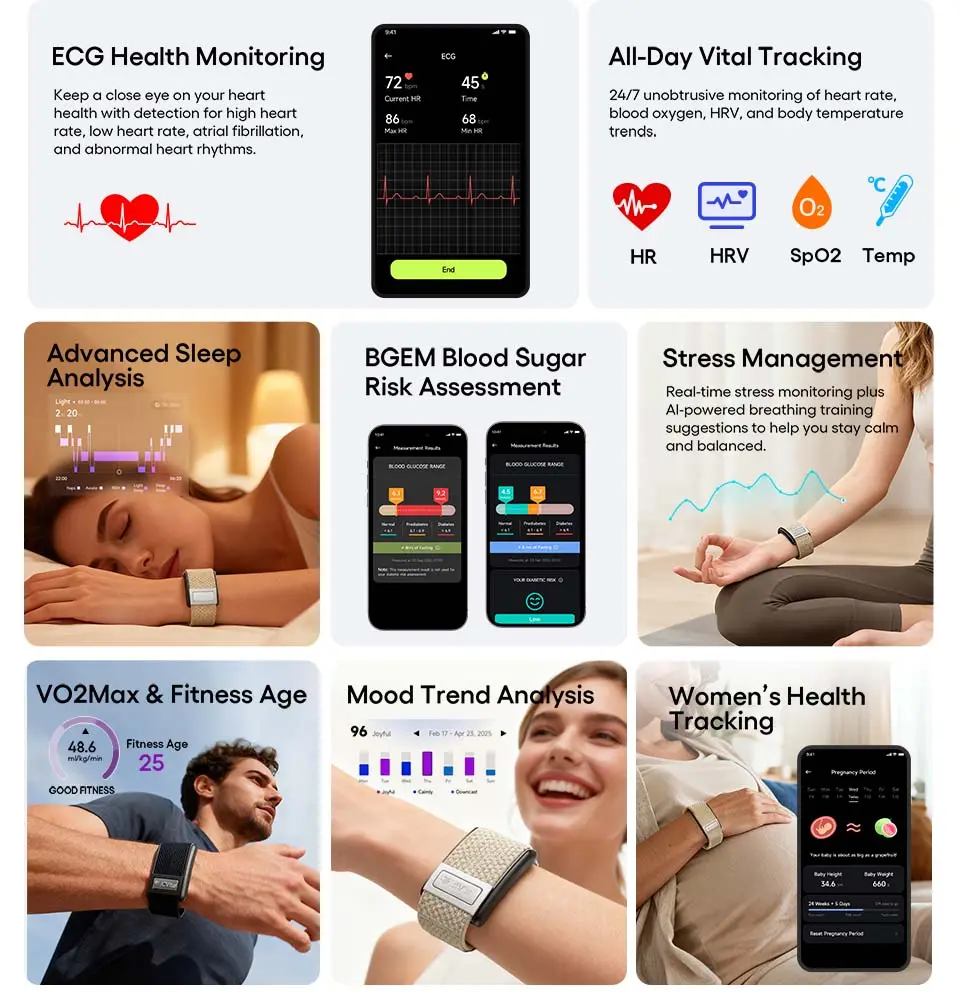
Example: JCVital V8 ECG Smart Band
The JCVital V8 ECG Smart Band exemplifies this category of medical-grade health monitoring devices. Key features include:
ECG Health Monitoring:
- Medical-grade sensor
- Comprehensive rhythm analysis: high heart rate, low heart rate, atrial fibrillation, and inconclusive rhythm detection
- Medical-quality ECG waveform export
- Abnormal rhythm alerts
Comprehensive Health Tracking:
- Continuous heart rate and HRV monitoring
- Blood oxygen (SpO2) measurement
- Detailed sleep analysis (stages, efficiency, recovery)
- Activity and fitness tracking
User-Friendly Design:
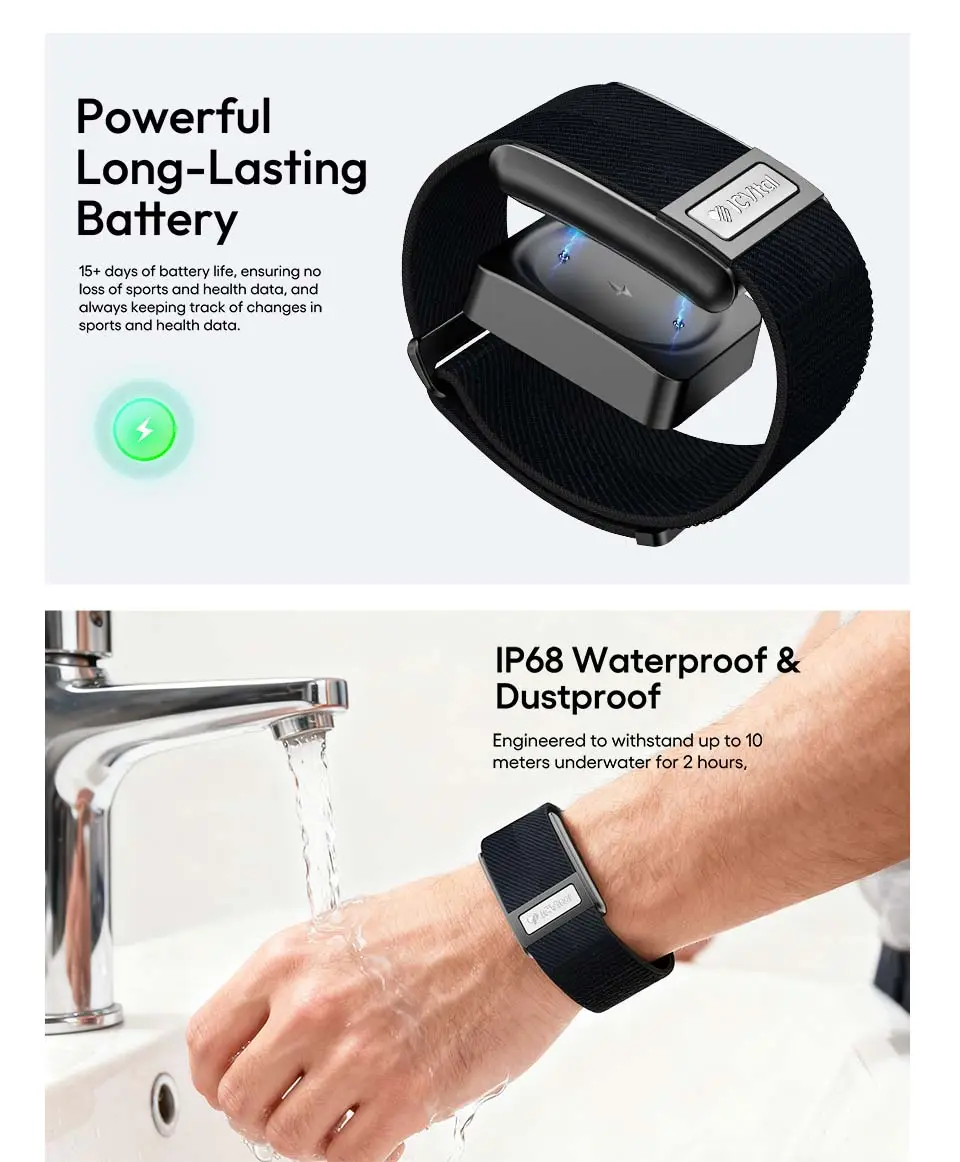
- Extended battery life supporting continuous monitoring
- Comfortable band suitable for 24/7 wear
- Intuitive app with clear health visualizations
- No subscription fees for full feature access
This represents the current state of accessible, medical-grade cardiac monitoring technology available to consumers.
Key Considerations for ECG Band Selection
Regulatory Clearance:
Verify medical certification for medical-grade ECG functionality. Devices marketed as "ECG-capable" without regulatory approval should be viewed as experimental.
Clinical Validation:
Look for published peer-reviewed studies validating device accuracy against clinical ECG standards.
Physician Integration:
Ensure ECG data can be easily exported and shared with healthcare providers in formats they can use for medical decision-making.
Comprehensive Monitoring:
Best value comes from devices combining ECG with robust continuous monitoring (PPG HR, HRV, SpO2, sleep) for holistic heart health assessment.
Total Cost of Ownership:
Evaluate not just device price but ongoing costs. Subscription-free devices provide better long-term value.
Understanding Your ECG Results
How to Take an Accurate ECG
Preparation:
Optimal Conditions:
✅ Sit comfortably with arm supported
✅ Relax—stress and movement cause artifacts
✅ Ensure good skin contact (clean, dry wrist)
✅ Remove from wrist momentarily and replace to refresh contact if needed
Avoid:
❌ Immediately after exercise (wait 5-10 minutes)
❌ While moving or talking
❌ With very cold hands (reduces signal quality)
Recording Technique:
- Position device correctly: Snug but comfortable on wrist
- Touch electrode: Place finger of opposite hand on device electrode/button
- Stay still: Remain motionless for 30-60 seconds
- Breathe normally: Don't hold your breath
- Wait for completion: Device will indicate when done
Signal Quality:
Most devices show real-time signal quality. If poor, adjust fit or finger position and restart.
Interpreting ECG Classifications
1. Normal Sinus Rhythm
Characteristics:
- Regular rhythm with consistent intervals
- Heart rate 60-100 BPM (at rest)
- Clear P-wave before each QRS complex
- Normal PR interval and QRS duration
Meaning:
Your heart's electrical system is functioning normally. No action needed unless you have symptoms.
Note:
"Normal" finding doesn't exclude all heart conditions (some require multi-lead ECG or echocardiography to detect).
2. Atrial Fibrillation
Characteristics:
- Irregularly irregular rhythm (no consistent pattern)
- Absent or unclear P-waves
- Varying R-R intervals
- May have rapid rate (>100 BPM) or controlled rate (60-100 BPM)
Meaning:
Upper heart chambers are quivering rather than contracting effectively. This is significant and requires medical evaluation.
Action Required:
- First detection: Contact physician within 24-48 hours (sooner if symptomatic)
- Known AFib: Document episode; discuss with cardiologist at next visit
- Persistent AFib: Requires ongoing medical management
Important:
AFib increases stroke risk 5-fold. Anticoagulation therapy dramatically reduces this risk.
3. High Heart Rate
Characteristics:
- Heart rate >100 BPM while resting
- May have regular or irregular rhythm
Possible Causes:
- Sinus tachycardia (normal response to stress, fever, dehydration)
- Atrial fibrillation with rapid ventricular response
- Supraventricular tachycardia (SVT)
- Anxiety or panic attack
- Hyperthyroidism
- Medication effects (decongestants, stimulants)
Action Required:
- Occasional, asymptomatic: Monitor; may be normal response
- Frequent or symptomatic: Medical evaluation recommended
- Sustained >150 BPM at rest: Seek medical attention same day
4. Low Heart Rate (Bradycardia)
Characteristics:
- Heart rate <60 BPM while awake
- May have regular rhythm
Possible Causes:
- Normal in athletes: High cardiovascular fitness
- Medications: Beta-blockers, calcium channel blockers
- Sick sinus syndrome: Heart's pacemaker malfunction
- Heart block: Electrical conduction delay
- Hypothyroidism: Low thyroid hormone
- Sleep apnea: Oxygen deprivation during sleep
Action Required:
- Asymptomatic, athletic: Likely normal; monitor
- Symptomatic (fatigue, dizziness, fainting): Medical evaluation needed
- Very low (<40 BPM while awake): Contact physician
5. Inconclusive
Characteristics:
- Algorithm cannot confidently classify rhythm
- May show irregular pattern not matching AFib criteria
- Signal quality adequate but rhythm unusual
Possible Causes:
- Premature atrial or ventricular contractions (PACs/PVCs)
- Other arrhythmias not in algorithm training
- Borderline rhythm patterns
- Artifacts mimicking arrhythmia
Action Required:
- Single inconclusive reading: Retake ECG when calm and rested
- Repeated inconclusive results: Share ECG with physician for expert interpretation
- Symptomatic: Seek medical evaluation regardless of classification
Important:
"Inconclusive" is a safety feature—device errs on side of caution rather than providing potentially incorrect classification.
6. Unreadable / Poor Signal
Characteristics:
- Excessive noise or artifacts
- Cannot identify cardiac waveforms clearly
Causes:
- Poor skin contact
- Movement during recording
- Loose band fit
- Very dry skin
- Electromagnetic interference
Action Required:
- Check device fit and skin contact
- Retake in calm, seated position
- Clean device sensors and skin
- If persistent, contact device support
Always Share:
✅ First-time AFib detection
✅ New or changing symptoms (palpitations, chest pain, dizziness, shortness of breath)
✅ Repeated inconclusive classifications
✅ Heart rate patterns that concern you
✅ Significant changes from your baseline
How to Share:
ECG PDF Export:
Most medical-grade ECG bands allow PDF export including:
- Full waveform
- Rhythm classification
- Heart rate
- Recording time/date
Methods:
- Email to physician's office
- Upload to patient portal
- Bring printed copies to appointment
- Share directly through health app integration
Context to Provide:
- Symptoms during recording (if any)
- Activities preceding recording
- Medications you're taking
- Recent changes in health status
Frequently Asked Questions
Q: Can ECG fitness bands diagnose heart attacks?
A: No. Single-lead ECG bands cannot diagnose heart attacks (myocardial infarction).
Why Not:
Heart Attack Diagnosis Requires:
- Multi-lead ECG (typically 12 leads) showing ST-segment elevation or depression in specific lead configurations
- Spatial information about which part of heart is affected
- Correlation with cardiac biomarkers (troponin blood test)
- Clinical assessment of symptoms
Single-Lead Limitations:
- Cannot show ST-segment changes reliably
- Lacks spatial resolution to locate infarction
- May show normal rhythm during/after some heart attacks
Important:
Heart Attack Symptoms:
- Chest pain/pressure (especially radiating to arm, jaw, back)
- Shortness of breath
- Nausea, lightheadedness
- Cold sweat
Action: Call emergency services immediately (911 in US). Do NOT rely on ECG band. Do NOT delay seeking emergency care to take an ECG.
What ECG Bands Can Show:
After a heart attack, ECG may show:
- Arrhythmias (common post-MI complication)
- Heart rate changes
- Q-waves (in some cases, weeks later)
But these are not diagnostic and require clinical correlation.
Q: How accurate are consumer ECG bands compared to medical ECG?
A: FDA-cleared consumer ECG bands demonstrate 95-99% accuracy for atrial fibrillation detection compared to clinical 12-lead ECG.
Detailed Accuracy Breakdown:
AFib Detection (Best Validated):
- Sensitivity: 95-99% (correctly identifies AFib when present)
- Specificity: 95-99% (correctly identifies normal rhythm)
- Comparable to clinical ECG for this specific rhythm
Other Arrhythmias:
- Less well-validated
- Can identify abnormalities but may not specify exact type
- Requires physician interpretation
Heart Rate Measurement:
- Extremely accurate: 99%+ accuracy
- Matches clinical ECG for rate
Waveform Quality:
- Single-lead provides less information than 12-lead
- Adequate for rhythm analysis
- Insufficient for comprehensive cardiac assessment (ischemia, chamber enlargement, etc.)
Comparison Table:
| Feature | Consumer Single-Lead ECG | Clinical 12-Lead ECG |
| AFib Detection | 95-99% accurate ✅ | 99%+ accurate (gold standard) |
| Heart Rate | 99%+ accurate ✅ | 99%+ accurate |
| Arrhythmia Classification | Basic types only | Comprehensive ✅ |
| Heart Attack Diagnosis | Not capable ❌ | Diagnostic ✅ |
| Electrical Conduction Detail | Limited | Comprehensive ✅ |
| Spatial Information | None (1 angle only) | Complete (12 angles) ✅ |
| Convenience | Immediate, anywhere ✅ | Requires medical visit |
| Cost | One-time device purchase ✅ | Medical billing |
Clinical Perspective:
Cardiologists increasingly recognize consumer ECG as valuable screening and monitoring tool but not replacement for clinical ECG when comprehensive diagnosis needed.
Q: Do I need to take an ECG every day?
A: Frequency depends on your medical situation and monitoring goals.
Recommended Frequencies:
Daily ECG:
Who:
- People with known paroxysmal AFib (intermittent episodes)
- Post-ablation monitoring (first 3-6 months)
- Those with frequent symptoms
- As directed by physician for specific monitoring
Benefit:
- Captures AFib burden (percentage of days with AFib)
- Documents rhythm stability
- Identifies patterns (time of day, triggers)
Weekly ECG:
Who:
- High-risk individuals (age >65, hypertension, heart disease)
- Asymptomatic screening
- General health monitoring
Benefit:
- Regular screening without excessive testing
- Establishes baseline
- Early detection of developing issues
Symptomatic ECG (As-Needed):
Who:
- People experiencing palpitations, dizziness, chest discomfort
- Those with occasional symptoms
Benefit:
- Captures rhythm during symptoms
- Provides diagnostic information for physician
- Correlates symptoms with objective data
Monthly or Less Frequent:
Who:
- Healthy individuals without risk factors
- Those using ECG for general wellness
Benefit:
- Periodic screening
- Minimal time investment
Important Considerations:
Over-Testing Concerns:
- Excessive ECG testing (multiple times daily without medical indication) may increase anxiety
- Can lead to false positives (finding abnormalities that would resolve on their own)
Battery Life:
ECG recordings consume battery. Daily ECGs may reduce device battery life from 14 days to 7-10 days.
Best Practice:
Follow your physician's recommendations. If no specific guidance, weekly screening ECG plus symptom-driven recordings is reasonable for most users.
Q: Can I use an ECG fitness band if I have a pacemaker or ICD?
A: Generally yes, but with important considerations.
Safety:
ECG fitness bands do NOT interfere with pacemaker or ICD function. The small electrical signals used for ECG recording are far too weak to affect implanted devices.
Accuracy Considerations:
Pacemaker Effects on ECG:
- Pacing spikes visible on ECG (sharp vertical lines before paced beats)
- May confuse automatic rhythm classification algorithms
- Device may classify paced rhythm as "inconclusive"
ICD Effects on ECG:
- Similar to pacemakers if pacing is active
- ICD therapies (shocks) won't be captured by wearable ECG
Appropriate Use:
Valid Applications:
✅ Monitoring heart rate trends
✅ Detecting AFib (if device has AFib detection capability despite pacemaker)
✅ Capturing symptoms between device checks
Limitations:
❌ Cannot assess pacemaker function (requires device interrogation by cardiologist)
❌ Automatic classification may be unreliable
❌ Waveform interpretation requires knowledge of paced rhythms
Recommendation:
Discuss with your cardiologist before using ECG band if you have implanted cardiac device. They can advise on:
- Whether ECG band adds value to your monitoring
- How to interpret results with paced rhythms
- What findings should prompt device check
Q: Will my ECG data be kept private?
A: Privacy protections vary by manufacturer. Key considerations:
Regulatory Frameworks:
HIPAA (United States):
Consumer health devices are generally NOT covered by HIPAA unless:
- Provided by your healthcare provider
- Data flows through covered entity (hospital system, physician practice)
Most direct-to-consumer ECG bands are NOT HIPAA-covered entities.
GDPR (Europe):
Stricter privacy protections apply:
- Health data classified as "sensitive personal data"
- Explicit consent required for processing
- Right to data deletion
- Right to data portability
What to Look For:
Privacy Policy Review:
✅ Where data is stored (cloud location, jurisdiction)
✅ Who has access to data (company employees, third parties)
✅ Data sharing practices (sold to advertisers? shared with insurers?)
✅ Retention policies (how long data is kept)
✅ Deletion rights (can you delete your data?)
Encryption:
✅ Data encrypted in transit (HTTPS, TLS)
✅ Data encrypted at rest (on servers)
✅ Local device encryption
Data Ownership:
✅ You retain ownership of health data
✅ Can export data in standard formats
✅ Can delete account and data
Third-Party Sharing:
❌ Red flag: Data sold to data brokers, advertisers
❌ Red flag: Sharing with insurance companies without explicit opt-in
✅ Good: No third-party sharing or only with explicit user consent
Best Practices:
Before Purchase:
- Read privacy policy (especially data sharing section)
- Search for news about company's data practices
- Check if company has had data breaches
During Use:
- Use strong, unique password
- Enable two-factor authentication if available
- Review privacy settings regularly
- Don't share more data than necessary (e.g., don't link unrelated accounts)
When Sharing with Physician:
- Use secure methods (encrypted email, patient portal)
- Share specific ECGs, not full account access
- Understand physician's data handling practices
Q: Can stress or anxiety cause abnormal ECG readings?
A: Yes. Stress and anxiety significantly affect heart rhythm and can cause ECG abnormalities.
Stress-Induced ECG Changes:
Sinus Tachycardia:
- Normal rhythm but rapid rate (>100 BPM)
- Most common stress response
- ECG shows normal waveforms, just faster
- Not pathological—appropriate physiological response
Premature Contractions:
- Stress increases PACs (premature atrial contractions) and PVCs (premature ventricular contractions)
- Felt as "skipped beats" or fluttering
- Usually benign but can make ECG "inconclusive"
- Very common during anxiety
Artifacts:
- Muscle tension creates electrical noise
- Trembling hands interfere with signal
- May make ECG unreadable
- Not a heart problem—recording quality issue
Anxiety-Specific Considerations:
Panic Attacks:
Can cause:
- Heart rate 120-180 BPM (sinus tachycardia)
- Hyperventilation affecting ECG baseline
- Chest pain (not cardiac origin but very real)
- Normal ECG during event (confirms not dangerous cardiac arrhythmia)
Health Anxiety:
- Excessive ECG testing can worsen anxiety
- Finding benign variations (PACs, PVCs) can trigger anxiety spiral
- May misinterpret normal variations as dangerous
Distinguishing Anxiety from Cardiac Issues:
Anxiety Characteristics:
- Triggered by stress/worry
- Associated with psychological symptoms (fear, worry, dread)
- Responds to relaxation techniques
- Normal ECG between episodes
Cardiac Arrhythmia Characteristics:
- May occur without emotional trigger
- No psychological symptoms
- Doesn't respond to relaxation
- Abnormal ECG pattern during episodes
Gray Area:
Some people have both anxiety AND cardiac arrhythmias. Anxiety can trigger cardiac arrhythmias in susceptible individuals.
Recommendations:
If Stress-Prone:
- Take ECG when calm, rested
- Practice relaxation before recording
- Don't obsess over every reading
- Discuss anxiety management with physician
When to Seek Help:
- Palpitations that are new, frequent, or severe
- Palpitations with chest pain, shortness of breath, fainting
- ECG showing AFib or other significant arrhythmia (regardless of anxiety)
Mental Health Matters:
Treating anxiety often reduces frequency of benign palpitations and improves quality of life.
Q: How long does the ECG band battery last?
A: Battery life varies by model and usage pattern:
Typical Battery Life:
Without ECG Use:
- Continuous heart rate (PPG) only: 10-21 days
- Depends on display usage, notifications, features enabled
With Regular ECG Use:
| ECG Frequency | Typical Battery Life |
| No ECG recordings | 14-21 days |
| 1 ECG per week | 13-20 days |
| 1 ECG per day | 10-14 days |
| Multiple ECG per day (3-5) | 7-10 days |
| Very frequent ECG (10+/day) | 5-7 days |
Battery Impact Factors:
ECG Recording:
- Each 30-second ECG uses ~0.5-1% battery
- Processing and AI analysis add consumption
- Syncing to phone adds consumption
Other Features:
- Display brightness and always-on settings
- Continuous SpO2 monitoring
- GPS tracking during exercise
- Frequent notifications
Battery Optimization Tips:
✅ Reduce display brightness
✅ Disable always-on display
✅ Limit notification frequency
✅ Turn off unused features (continuous SpO2 if not needed)
✅ Take ECGs only when medically indicated, not excessively
✅ Keep firmware updated (often includes battery optimizations)
Charging:
- Typical charge time: 1-2 hours
- Magnetic or proprietary charging cable
- Charge weekly for most users (Sunday night routine)
Conclusion
ECG technology in fitness bands represents a significant advancement in consumer health monitoring, bringing medical-grade cardiac screening to millions of people. For individuals with known heart conditions, high risk factors, or unexplained symptoms, these devices provide valuable data that can guide medical care and potentially save lives through early detection of dangerous arrhythmias like atrial fibrillation.
Key Takeaways:
✅ ECG and optical heart rate serve different purposes: PPG monitors continuously; ECG provides diagnostic snapshots
✅ FDA clearance matters: Medical-grade devices have proven accuracy; recreational "ECG" features may not
✅ AFib detection is the killer app: Single-lead ECG excels at identifying this common, dangerous, often asymptomatic condition
✅ Know the limitations: Consumer ECG cannot diagnose heart attacks or replace comprehensive clinical evaluation
✅ Share data with physicians: ECG bands are most valuable when integrated into medical care, not used in isolation
✅ Match device to need: High-risk individuals benefit most; healthy young adults with no symptoms may not need ECG functionality
✅ Balance monitoring with anxiety: Excessive testing can create health anxiety; focus on medically appropriate frequency
The integration of ECG technology into affordable, wearable devices has democratized cardiac monitoring in a way unimaginable a decade ago. As algorithms improve and regulatory frameworks mature, these devices will play an increasingly important role in preventive cardiology and chronic disease management.
For those considering an ECG fitness band, the decision should be guided by medical need, risk factors, and physician recommendations—not marketing hype. When used appropriately, these devices serve as powerful tools for heart health awareness, early disease detection, and peace of mind.
Additional Resources:
- American Heart Association: Comprehensive cardiovascular health information (heart.org)
- Heart Rhythm Society: Patient education on arrhythmias (hrsonline.org/patient-resources)
- CDC Heart Disease Information: Public health guidelines (cdc.gov/heartdisease)
- FDA Medical Device Database: Verify device clearance status (accessdata.fda.gov/scripts/cdrh/devicesatfda)
Medical Disclaimer:
This guide provides educational information about ECG fitness band technology. It is not medical advice. Always consult qualified healthcare providers for diagnosis, treatment, and medical decisions. ECG fitness bands are screening tools, not replacements for clinical care. If you experience cardiac symptoms (chest pain, severe palpitations, fainting, shortness of breath), seek immediate medical attention—do not rely on wearable device data.
This guide was last updated in January 2026. ECG technology and regulatory approvals evolve rapidly—verify current device certifications and capabilities before purchase.
Related Articles:
What Is ECG and How Is It Used in Wearables? A Complete Guide for 2026
How ECG Wearable Devices Work: Technology, Algorithms & Real-World Applications
PPG vs ECG: Which Is More Accurate? A Deep Dive Into Global Wearable Health Monitoring Technologies
About the Author

Kyler is a senior content marketing specialist at J-Style(Jointcorp|Joint Chinese Ltd | Youhong Medical), a leading smart ring, smart band, and smart watch manufacturer and supplier in China. With 8 years of experience in the wearable tech industry, he creates professional content for global B2B buyers seeking reliable factory, wholesale, OEM/ODM, and SDK/API solutions. At J-Style, Kyler focuses on helping partners understand the value of high-quality Chinese smart wearables and how J-Style’s innovative manufacturing capabilities support scalable business growth.






